Portal Hypertension
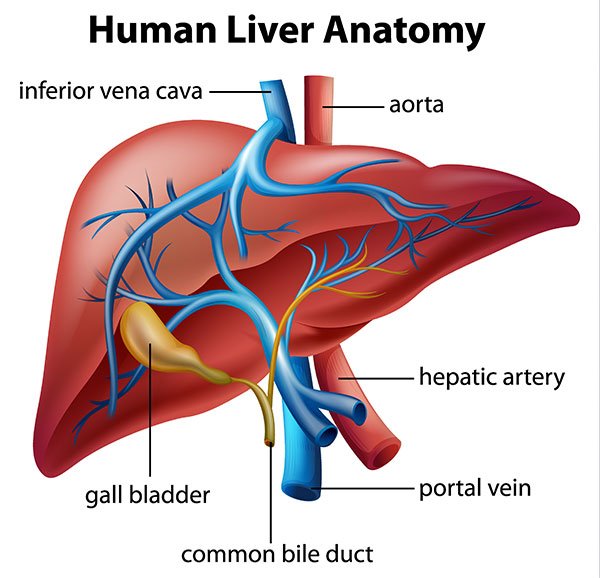
Portal hypertension is high blood pressure of the portal vein. The portal vein, a major vein in the abdomen, collects nutrient-rich blood from the intestines and delivers it to the liver to nourish it, where it is purified for the body to use.
What is Portal Hypertension?
Portal hypertension is high blood pressure of the portal vein. The portal vein, a major vein in the abdomen, collects nutrient-rich blood from the intestines and delivers it to the liver to nourish it, where it is purified for the body to use.
Like other organs, the liver needs oxygen and nutrients to function, which it receives from the portal vein. After the oxygen-rich and nutrient-rich blood passes through the liver, it flows into the hepatic veins and into the inferior vena cava, which takes it back to the heart. Blocked or reduced blood flow at any point of this process will result in increased pressure inside the portal vein. When this occurs, blood is detoured into other smaller veins that ultimately allow blood to flow back to the heart. However, these smaller veins can enlarge and form varices (varicose or dilated veins).
The most common cause of portal hypertension is cirrhosis, which refers to the “hardening” of the liver because of scar tissue. The other primary cause of portal hyper-tension is due to clots which narrow or block blood flow through the veins to and from the liver. Portal hypertension is fairly uncommon, but when it occurs, it most often occurs in older adults and may result in death, if untreated.
Symptoms
Ascites (fluid build-up in the abdomen)
Weight loss (malnutrition)
Enlarged liver (at times)
Varicose veins of the esophagus (varices) – with possible bleeding
Jaundice (yellowing of the skin)
Causes
Cirrhosis of the liver (may be due to alcohol use or hepatitis)
Clotting of the PORTAL vein
Clotting of the hepatic veins
Varices can rupture or burst, especially where the esophagus and the stomach join. Bleeding from varices can be massive, causing patients to vomit blood, which is a major cause of death in patients with portal hypertension.
Blood may also be detoured through the veins along the rectum, the lowest portion of the large intestine (colon), causing them to enlarge. Enlarged veins along the rectum are called internal hemorrhoids, which can rupture and result in massive bleeding from the rectum and anus.
Another symptom of portal hypertension is ascites, the collection of large amounts of fluid in the abdomen. Ascites can lead to early sensations of being full when eating, resulting in malnutrition. People with ascites often have a harder time being active because of the weight of the fluid and the large size of their abdomen. Someone with massive ascites will have a protruding or swollen abdomen, often with thin legs and arms, due to muscle loss because of liver disease and malnutrition.
Ascites can cause the kidneys to fail. Urgent steps must be taken to drain the ascites and to monitor the kidneys and liver. Unless the liver function is corrected and the kidneys recover, approximately half of these patients die within a few weeks.
Diagnosis
Unfortunately, there is no simple way or test to show if a person has portal hypertension. We cannot use a blood pressure cuff like we can on an arm to measure “whole body” hypertension. Doctors become aware of portal hypertension when its signs and symptoms are first noticed. Imaging and laboratory tests suggest cirrhosis, which can be further diagnosed by a liver biopsy.
Some patients who undergo a biopsy will also have special pressure measurements taken in the liver at the same time to diagnose portal hypertension. Many of the imaging studies such as CT, MRI and ultrasound can also show signs of portal hypertension such as varices and enlargement of the spleen.
Treatment
Medical treatment of portal hypertension includes betablockers, which are known to many as drugs to improve blood pressure and heart function. This class of drugs helps to decrease blood flow into the portal-vein system, decreases pressure and reduces the risk of bleeding from varices.
Minimally invasive procedures such as endoscopic variceal sclerotherapy (EVS), which involves the injection of a solution to seal the bleeding, and endoscopic variceal banding (EVB), which is the placement of a band from inside the esophagus to seal the bleeding, are used to stop bleeding from varices.
Another solution is a procedure known as transjugular intrahepatic portasystem shunt (TIPS). This procedure inserts a stent (a hollow wire tube) between a hepatic vein and a branch of the portal vein. The stent passes through the liver to connect these two vascular structures. With TIPS, blood moves through the stent and bypasses the liver. This procedure has both advantages and disadvantages. TIPS reduces portal-vein pressure and bleeding from varices. However, because some blood bypasses the liver, some wastes are not cleared from the bloodstream. These nitrogen-containing compounds can cause confusion, which has to be treated with medications.
Some health professionals feel that there is no proof that someone lives longer after the TIPS procedure, that it is expensive and has a high failure rate within one year because the stent often becomes narrowed or blocked. Other professionals believe that TIPS is the definitive lifesaving procedure for acute massive variceal hemorrhage at many institutions. While the TIPS procedure may be expensive, it is no more so than the other procedures described. TIPS did have a failure rate, but that is for the most part historical and misleading. Today TIPS is done with covered stents and patients are followed with ultrasound for restenosis. While many patients that have uncovered stents will have restenosis, this is caught on a surveillance program and easily remedied with balloon angioplasty.
Risk Factors
Coming Soon!
Resources
Be The Voice For Patients Like You!
Vascular Cures is inviting patients and advocates to share their stories, advise on our programs, and help us advocate for patient needs. Patients as Partners is a community where patients are heard, empowered, and encouraged to impact the health system. Learn more and request more information here.