Deep Vein Thrombosis
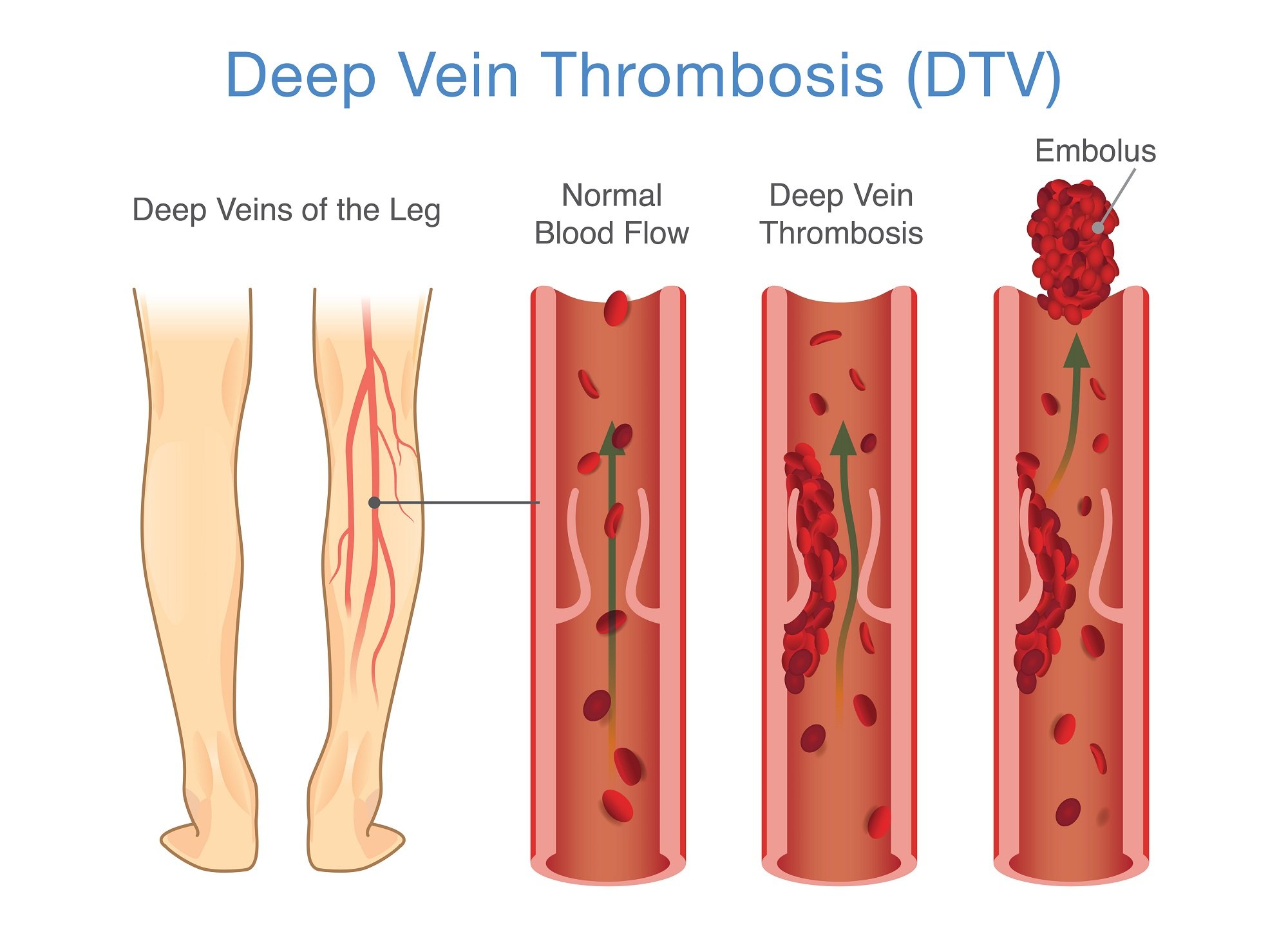
Deep Vein Thrombosis (DVT) occurs when a blood clot develops in the large veins of the legs or pelvic area.
What is Deep Vein Thrombosis (DVT)?
Deep vein thrombosis (DVT) happens when a blood clot (also known as a thrombus) forms in a large vein. These clots usually develop in the legs or pelvic area. Some DVTs don’t hurt, but others can be quite painful. With quick diagnosis and treatment, most DVTs are not life-threatening. However, they can be dangerous. A clot that forms in the large, deep veins is more likely to break free and travel through the bloodstream. This is called an embolus. When an embolus travels from the legs or pelvis and gets stuck in a lung artery, the condition is known as a pulmonary embolism (PE). This is a potentially deadly condition and needs immediate medical treatment.
Common Signs and Symptoms of DVT
Some people with a DVT never develop symptoms. For those who do, the symptoms can develop slowly or suddenly. If you have any of these symptoms in your legs or pelvic area, contact your health care provider immediately:
Sudden swelling of the leg
Pain or tenderness which you may feel when standing or walking
Skin that is warm to the touch in the leg that is painful
Fullness or firmness of the veins just beneath the skin
Change in skin color that appears red or discolored
Common Signs and Symptoms Pulmonary Embolism
PE can be fatal. If you experience any of these symptoms, seek medical attention right away:
Unexplained shortness of breath
Sudden chest pain with deep breathing
A sudden, unexplained sense of anxiety
Sudden collapse
Sweating
Bloody phlegm (coughing up blood or bloody mucus)
The signs and symptoms of DVT and PE are different for each person. For example, changes in skin color can vary depending on racial or ethnic backgrounds. Some individuals may also experience uncommon symptoms such as dizziness, back pain, or wheezing.
Diagnosis
Providers usually use an ultrasound exam to diagnose DVT. This simple, painless test is safe and widely available. You may also need to get a blood test that measures “D-dimer,” a sign of recent clotting.
Treatment
Medication
Both DVT and PE are treated with blood thinners that require a prescription. These medicines, called anticoagulants, make it harder for your blood to clot and can stop clots from getting bigger. They may also prevent new clots from forming and lower the risk for a PE. However, they do not break up existing clots. The body’s natural systems will do its best to dissolve the clots over time.
Compression
Sometimes, patients with DVT need to wear compression stockings. Compression stockings can also be used to prevent DVT. The stockings help treat swelling and prevent skin changes that can develop over time due to post-thrombotic syndrome, a condition marked by:
Dermatitis (redness, irritation, or swelling of the skin)
Skin discoloration
Scarring
Ulcers (or open sores)
Your provider may also recommend a sequential compression device (SCD). This device uses air pressure to inflate long leg cuffs, which massages the legs to increase blood flow and lower the risk for blood clots.
Thrombolysis
If you’re at high risk or have a life threatening situation, your health care provider may recommend a catheter-directed thrombolysis. With this procedure, a provider threads a catheter (a small, flexible tube) up through the clot and then injects a special drug to dissolve the blockage. The catheter has many tiny holes so that the “clot-buster” drug can reach the entire area of the DVT. Think of it like a soaker hose that has lots of side holes to distribute water across the yard. Sometimes, a tiny vacuum cleaner is then used to suck out the softened clot. Once the clot is gone, the provider may need to insert a small balloon or stent (a tiny tube) to open the narrowed vein. This extra step is typically used only in the iliac veins, located in the pelvic area. With thrombolysis, the patient will also need anticoagulant medication (heparin) to prevent new blood clots from forming while the existing clot is being dissolved.
Vena Cava Filter
If you can't take blood thinners or they're not working well, your doctor may recommend a vena cava filter. The filter is inserted inside a large vein called the vena cava. The filter catches blood clots before they travel to the lungs, which prevents pulmonary embolism. However, the filter doesn't stop new blood clots from forming.
Surgery
For the few patients who cannot take clot-dissolving drugs, the provider may recommend surgical thrombectomy which is the removal of the clot through a small incision at the groin. However, this procedure involves extra risk and costs more money. Surgical clot removal is usually only recommended for active, healthy patients who have major clots higher up in the leg. It can significantly reduce the complications of DVT, such as chronic leg swelling, discoloration, and ankle ulcers. But it does come with an increased risk for serious bleeding. You’ll need to meet with a vascular specialist to find out if this approach is right for you.
Tips to Lower Your Risk for DVT
Elevate your legs when you are sitting for extended periods of time.
While on an airplane for more than four hours, stand up and walk in the aisles every hour or so. In your seat, pump your feet up and down. Also, ask your health care provider if you should wear compression stockings when you travel.
If you are flying, drink plenty of nonalcoholic beverages.
Stay hydrated: Drink at least six glasses of water a day.
Ask your healthcare provider if you’re at risk for DVT and need to take medication.
If you have varicose veins, wear support hose (especially if you’re pregnant).
Do not wear constricting clothing around the legs or waist. Avoid elastic bands and tight-fitting socks.
Risk Factors
Slow or sluggish blood flow
Tendency for a person’s blood to clot quickly
Irritation, inflammation, or injury to a vein
Recent major surgery (especially hip/knee)
Congestive heart failure
Excess weight
Chronic respiratory failure
A history of smoking
Varicose veins
Pregnancy
Estrogen treatment
Smoking
Resources
Be The Voice For Patients Like You!
Vascular Cures is inviting patients and advocates to share their stories, advise on our programs, and help us advocate for patient needs. Patients as Partners is a community where patients are heard, empowered, and encouraged to impact the health system. Learn more and request more information here.