Lymphedema
Lymphedema is a common cause of leg or arm swelling due to the collection of too much lymph fluid. Nearly one million Americans are affected by this condition.
What is Lymphedema?
Although many people have never heard of this condition, lymphedema is a common cause of leg or arm swelling due to the collection of too much lymph fluid. Nearly 1 million Americans are affected by this condition, and the number of people worldwide with it may soon approach 100 million. The swelling produced by lymphedema is usually not painful, but it may cause a heavy, aching discomfort and limit a person’s ability to use his or her arms or legs, increase the risk of certain infections, or cause emotional distress due to the severe swelling of the arm or the leg.
Causes
There are three types of blood vessels in the body: arteries, veins, and lymph vessels. Arteries deliver oxygen and nutrient-rich blood from the heart to the tissues and organs of the body and the veins return blood back to the heart to be re-oxygenated by the lungs. The lymph vessels are a third type of blood vessel that carries fluid from the tissues and organs of the body back to the veins. The lymph vessels are long, thin-walled tubes that form a very intricate network in the arms and the legs. In some cases, these lymph vessels are absent or are damaged or destroyed, and lymph fluid accumulates in the tissues of the arm or leg causing severe swelling.
Many things can damage the lymph vessels and cause lymphedema, including cancer and treatment for cancer, such as surgery or radiation therapy, infections, other surgical procedures, and certain injuries. In some cases, lymphedema is an inherited condition that is present at birth or develops during the early years of life or puberty. In these inherited cases, there is commonly a family member who also had lymphedema. In the United States, treatment for breast cancer, including surgery and radiation therapy, is one of the most common causes of lymphedema. Interestingly, the most common cause of lymphedema worldwide is a certain type of infection known as filariasis.
Symptoms
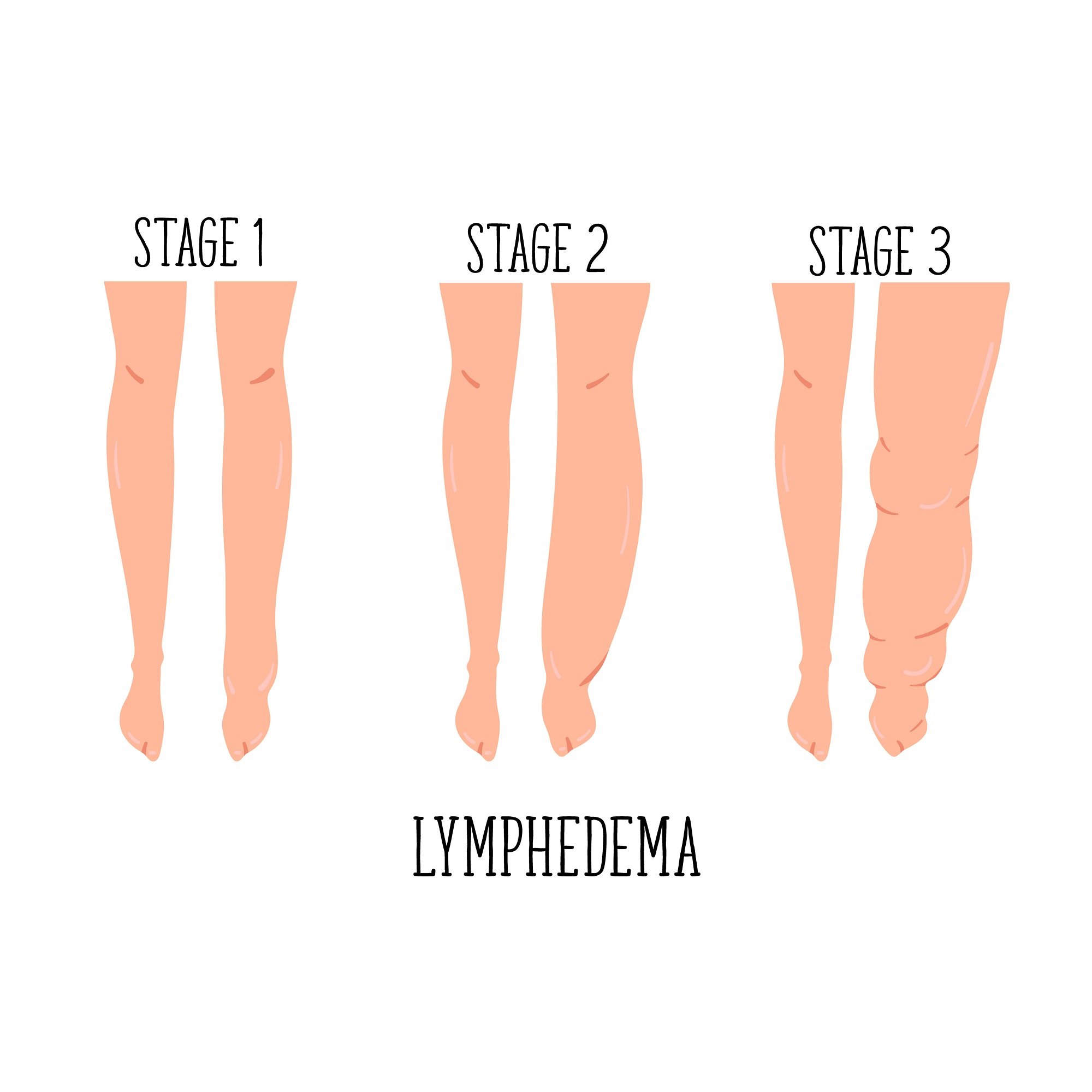
Lymphedema usually manifests as severe swelling of an arm or leg. For patients who have developed lymphedema as a complication of cancer treatment, the swelling is almost always on the same side as the treatment. In some cases, lymphedema may involve both of the limbs, typically the legs. The swelling commonly extends from the arm or leg into the fingers or the toes. In the early stages of lymphedema, the swelling is soft, and pressing on the limb may result in movement of the fluid. This is called “pitting edema.” In the later stages of lymphedema, scar tissue and fibrous tissue may develop in the swollen limb causing a more dense texture of the swelling and a cobblestoned or orange-peel like appearance of the skin. Patients with lymphedema may experience heaviness of the effected arm or leg and have difficulty with exercise or participation in other activities. In the most severe cases of lymphedema, swelling may be disfiguring and may lead to emotional distress and even difficulty wearing clothes or shoes.
In addition to swelling, patients with lymphedema are at risk for developing certain types of skin infection in the swollen arm or leg known as cellulitis and lymphangitis. In mild to moderate infections, the skin will become warm, red, tender and the patient may feel flu-like symptoms. Oral antibiotics and careful skin care should be started as soon as symptoms develop. In severe cases, high fevers and even shock may develop and require immediate hospitalization for intravenous antibiotics and close observation. Patients with severe, long-standing lymphedema are at increased risk for developing certain types of cancer, including certain skin cancers and lymphoma, although this is very rare.
Diagnosis
Lymphedema is generally diagnosed on the basis of medical history and physical examination. Lymphedema must be differentiated from other causes of limb swelling, including venous insufficiency, deep vein thrombosis (blood clot), congestive heart failure, other medical conditions such as kidney, liver, or thyroid disease, and enlargement of the legs due to extra fat (called lipidema). In some cases, additional diagnostic testing is necessary, such as a lymph scan known as lymphoscintigraphy. Lymphos cintigraphy can be used to detect blockages in the lymph vessels or the absence of lymph vessel. This test requires a small amount of radioactive material to be injected through a small needle into the hand or foot. Except for minor discomfort, this test is not otherwise dangerous or painful. Other tests may be performed to exclude the other causes of leg swelling, such as a CAT scan or MRI, blood tests, or an ultrasound to exclude the presence of a blood clot.
Treatment
Lymphedema is a chronic condition that can be diagnosed by a healthcare provider. There are many effective treatments of lymphedema. Although it is unusual to completely cure lymphedema, most people who receive proper treatment can lead normal, active lives.
The most important therapy for lymphedema is wearing compression garments such as prescription-strength stockings or gloves or short-stretch bandages. These compression garments need to be worn daily, but should be removed at night. They provide adequate compression for the treatment of lymphedema, and these garments must be prescribed by a healthcare provider.
Probably the most effective treatment for reducing swelling due to lymphedema is known as complete decongestive physiotherapy that involves a combination of therapeutic massage (known as manual lymphatic drainage) and the use of compression bandages. Complete decongestive physiotherapy involves intensive treatment over a limited period of time, such as multiple treatments per week for two or three weeks. At the end of therapy, a compression stocking or glove is fitted for long-term maintenance. In some cases, a healthcare provider may provide a pneumatic compression pump that is used on the arms or legs at home for additional treatment of lymphedema.
In rare cases, surgical treatment may be recommended for patients with advanced lymphedema that has not responded to complete decongestive physiotherapy and compression therapy. It is very unusual for lymphedema to require surgical treatment, and this should be performed only in experienced centers.
Personal Care
Personal hygiene and avoidance of injury are essential in the prevention of lymphedema-related problems, especially skin infection. Follow these simple personal care measures to help keep skin healthy and reduce the risk of infection or swelling to worsen:
Keep skin as clean as possible. Dry skin thoroughly, but gently, especially between toes.
Wash hands frequently, applying lotion after each hand-washing to avoid over-drying the skin.
Wear compression support garments as prescribed during waking hours, removing for sleep. Perform skin care before and after use. Wash gently and hang to dry; have spare garments for alternate use.
Avoid blood pressure cuffs, needle sticks, injections, or procedures on the affected limb. Wear a “lymphedema alert” bracelet.
Immediately report any new swelling or signs of infection such as redness, pain, warmth, streaks, rash, blisters, fever or flu-like symptoms.
Avoid tight clothing.
Avoid excess heat – overly hot showers, sun, hot tubs/saunas. Avoid sunburn and keep as cool as possible in summer weather.
Wear cotton-lined household gloves for housework; use garden gloves for gardening.
Carefully trim nails; see a podiatrist if necessary. Check feet with a mirror for wounds, fungal infections or cracked skin. Wear extra-wide, extra-depth shoes.
Avoid trauma – pet scratches, insect bites, burns, sports injuries, or bruising. Seek appropriate care immediately. Wash all cuts with soap and water and apply antibiotic ointment.
Maintain normal body weight. Follow a low-fat, low-salt, high-fiber diet plan. Exercise daily as ability allows – walking, swimming, light aerobics, biking, yoga and stretching are recommended.
*Excerpted from Lymphedema: A Patient’s Guide by Patricia A. Lewis, MSN, FNP, Bassett Healthcare, 1 Atwell Road, Cooperstown, NY 13326. Used with permission by the author.
Risk Factors
Cancer treatment, particularly lymph node dissection at the time of mastectomy for breast cancer and radiation therapy for breast, prostate or other cancers, are risk factors for the development of lymphedema in the future. Other risk factors include major trauma or burns, a family history of lymphedema, and exposure to filarial infection, which is a mosquito-borne illness common in Asia and Africa.
Resources
Be The Voice For Patients Like You!
Vascular Cures is inviting patients and advocates to share their stories, advise on our programs, and help us advocate for patient needs. Patients as Partners is a community where patients are heard, empowered, and encouraged to impact the health system. Learn more and request more information here.